What Is Medical Transcription Software? How AI Scribes Improve Accuracy, EHR Integration, and Patient Care
AI medical transcription software is transforming healthcare in 2025. Today's platforms offer instant documentation, automatic coding, complete HIPAA protection, and smooth EHR integration. These intelligent AI tools cut down paperwork, reduce physician exhaustion, and enhance the standard of patient care. In this article, we'll discover how AI scribes streamline workflows and provide precise, protected documentation.
.jpg)
Medical transcription has consistently been the foundation of healthcare documentation. It converts verbal dictation into organized patient records. Previously, experienced transcriptionists manually processed physician recordings, consultations, and clinical observations with strong accuracy. Now, AI medical transcription is revolutionizing this workflow with automation, speed, and real-time documentation.
Traditional transcription typically required 24 to 72 hours and averaged $1.50 to $5.00 per minute of audio. In contrast, AI medical transcription software finishes the same task in minutes while cutting costs by up to 60%. The global medical transcription industry is expected to expand from $58.3 billion in 2025 to $106.4 billion by 2035, growing at a compound annual growth rate (CAGR) of 6.2%.
This blog examines how AI medical transcription software is revolutionizing healthcare documentation in 2025.
What Is Medical Transcription Software?
Medical transcription software is a healthcare documentation tool that converts spoken medical dictation into accurate, written clinical notes. Physicians use it to document patient visits, diagnoses, and treatment plans.
Traditionally, doctors relied on human transcriptionists. They recorded notes using medical dictation software or digital devices, and transcriptionists typed reports manually. While effective, this method often delays documentation by 24–72 hours and adds significant costs.
How Does Medical Transcription Software Work?
Step 1: Capture Audio
Traditional medical transcription platforms record dictation from single-use devices or apps. They accept multiple audio formats, allow file tagging, and support playback controls.
Step 2: Manual Transcription
Human transcriptionists type reports while using medical dictionaries, hotkeys, or foot pedals. This ensured accuracy but also introduced delays and human error.
Step 3: Delivery and Integration
Completed transcripts are delivered through secure email, fax, or uploaded directly into EHR systems. This helped keep records accurate but required hours of admin work.
How AI Medical Transcription Software Works
AI has transformed this process. AI medical scribes and ambient AI scribe tools now listen during consultations and generate real-time clinical documentation.
Key advancements include:
- Speech-to-text medical transcription powered by voice recognition healthcare tools
- Automated medical note-taking with SOAP note templates
- EHR integration for seamless workflow
- HIPAA-compliant transcription with encryption and SOC2/ISO27001 medical software compliance
- Multilingual medical transcription to support diverse patient populations
Unlike traditional methods, AI vs traditional medical transcription shows clear advantages: faster turnaround, lower cost, and reduced physician burnout.
Top Features of Modern Medical Transcription Platforms: What ScribeHealth.ai Covers
Modern medical transcription software has advanced far beyond simple speech-to-text tools. Today’s platforms combine AI medical transcription, clinical documentation automation, and enterprise-grade security to give providers faster, more accurate, and safer workflows.
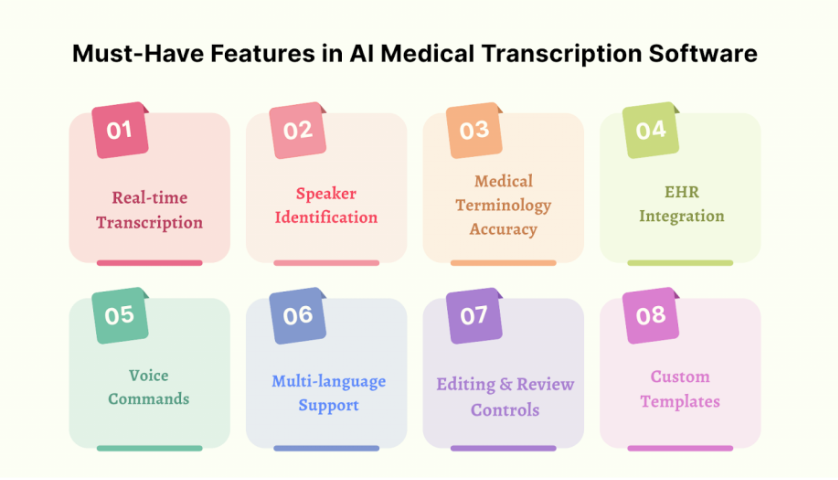
1. Real-Time AI Transcription & Ambient Voice Recognition
Imagine talking naturally with your patient while every word is instantly transformed into structured notes without pausing, typing, or backtracking. That’s the power of ambient AI scribe technology built into ScribeHealth.ai. Accuracy rates reach 98% for general terms and 95% for specialty-specific language, so providers can trust that the notes they review are clear and correct. The result? Less time editing, more time connecting with patients.
2. Automated Medical Coding & Billing Integration
Coding is one of the biggest pain points in healthcare. ScribeHealth.ai solves this by including automated ICD-10, CPT, and HCPCS coding at no extra cost. With up to 99% accuracy, providers see fewer billing errors, faster reimbursement, and stronger revenue capture. On average, practices report a 25% drop in claim denials and annual savings topping $150,000.
3. Comprehensive EHR Integration
Every practice runs differently, which is why ScribeHealth.ai offers flexible EHR integration across 35+ systems like Epic, Cerner, DrChrono, and eClinicalWorks. Options include simple Chrome extensions, advanced API integrations, and direct database connections, all HL7/FHIR compliant. In many cases, providers can be up and running within a week. Notes flow straight into the right fields, tasks sync automatically, and workflows finally feel seamless.
4. Enterprise-Grade Security
In healthcare, trust begins with data protection. ScribeHealth.ai is fully HIPAA compliant and backed by SOC2 Type II and ISO27001 certifications. Every audio file is encrypted with AES-256—the same security standard used by banks and deleted immediately after transcription. With global compliance frameworks including GDPR and PIPEDA, ScribeHealth.ai ensures providers can focus on patients, knowing their data is always safe.
5. Multi-Platform Accessibility & Offline Support
Documentation doesn’t stop when connectivity does. ScribeHealth.ai runs on desktops, tablets, mobile devices, and even integrates with telehealth video platforms with multi-platform medical transcription support. Its offline transcription mode keeps workflows uninterrupted in low-bandwidth or rural settings, syncing notes automatically when internet access returns.
6. Specialty-Specific Templates & Customization
Every specialty has unique needs. ScribeHealth.ai offers over 50 medical transcription templates across 56 specialties, from SOAP and DAP notes in primary care to therapy session summaries in psychiatry and pediatric growth charts. Its Smart Edit™ technology learns individual provider preferences, ensuring notes reflect each clinician’s unique style while maintaining compliance.
7. Analytics, Insights & ROI Tracking
ScribeHealth.ai provides advanced clinical workflow analytics. Practice managers can track time saved, productivity gains, and revenue opportunities in real time. Error tracking and gap analysis prevent mistakes before they impact billing or patient care. Built-in ROI calculators show exactly how the software improves profitability.
8. Competitive Pricing with a Free Tier
Affordability is another area where ScribeHealth.ai stands apart. The platform offers 20 free sessions per month, plus unlimited transcription at $49 per provider per month. Compared to traditional medical scribe software that costs $99–$150+, providers see 50–60% cost savings while gaining advanced features like built-in coding and broad EHR integration.
Benefits for Clinical Workflows
AI-powered medical scribe software is designed to ease one of the biggest challenges in healthcare: documentation. These tools free up valuable time for providers and create more space for patient interaction by automating note-taking and integrating directly with EHR systems.
One of the biggest advantages is the ability to reduce documentation time by one to two hours each day. Instead of typing notes after hours or struggling with manual dictation, clinicians can finish their records before leaving the office. This directly helps eliminate the administrative burden that fuels physician burnout, giving doctors back the time they need for rest or family.
Another key benefit is improved quality of care. With less typing and fewer computer distractions, providers can spend more time making eye contact, listening, and engaging in meaningful conversations. AI-powered real-time medical transcription ensures that notes are generated instantly, allowing workflows to run smoothly across different specialties.
These platforms also help streamline clinical workflows through automated note generation. Tasks such as referrals, follow-up reminders, and coding suggestions can be handled automatically, ensuring nothing falls through the cracks.
Finally, the cost savings are significant. Unlike traditional transcription services that charge per audio minute, most AI medical transcription platforms use subscription models. These plans are often cheaper than traditional transcription, delivering measurable ROI while improving both accuracy and efficiency.
Why ScribeHealth.ai Leads the Market
ScribeHealth.ai combines everything modern clinicians expect:
- Real-time AI transcription with ambient listening
- Built-in coding automation that accelerates billing
- Deep EHR integration across 35+ platforms
- Global compliance for HIPAA, GDPR, and SOC2 standards
- Cross-device documentation with offline capability
- Competitive pricing with a generous free plan
This means more accurate notes for providers, less time spent on admin, and more focus on patient care. In short, ScribeHealth.ai is more than a transcription tool. It’s a full clinical documentation software designed to streamline workflows and protect both patients and providers.
Conclusion
AI-powered medical transcription software makes documentation faster, safer, and more accurate. It gives clinicians the support they need to focus on what matters most by reducing admin burden and improving patient care time.
Ready to experience the difference? Try a HIPAA-compliant AI medical scribe today and streamline your clinical workflows

