Emergency Department AI Scribing: Capturing Critical Notes Under Pressure
If you're an emergency physician battling endless documentation, AI medical scribes for emergency departments offer real relief. These smart tools capture notes instantly, integrate with workflows, and transform chaos into efficiency. ScribeHealth leads with emergency-optimized features, helping you focus on saving lives while handling paperwork seamlessly.
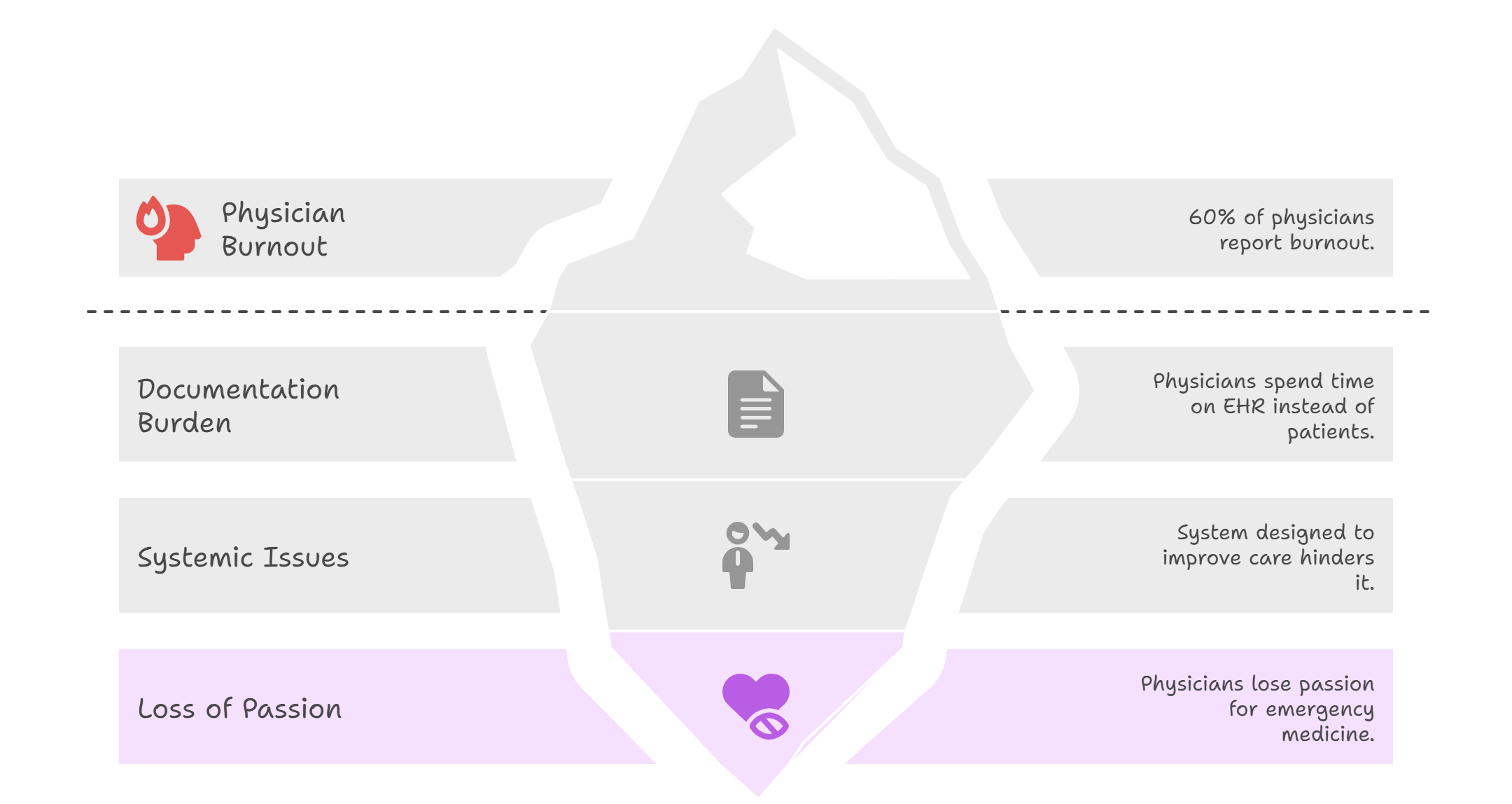
If you're an emergency physician, you know the crushing weight of documentation that follows every patient encounter. You're not alone in this struggle—60% of emergency physicians report burnout, the highest rate among all medical specialties. The very system designed to improve patient care has become your biggest obstacle to providing it.
You entered emergency medicine to save lives, not to spend precious minutes wrestling with electronic health records while patients wait. The solution you've been searching for is here: AI medical scribes for emergency departments. These intelligent systems eliminate documentation burdens, restore your focus to patient care, and help you reclaim the passion that brought you to emergency medicine in the first place.
What Is an AI Medical Scribe—and Why Does Emergency Medicine Need One?
Emergency departments face unique documentation challenges that traditional scribing solutions can't address. AI medical scribes offer 24/7 availability and instant processing capabilities that match the pace of emergency care.
The Emergency Department Documentation Crisis
Emergency medicine pushes doctors to their limits every single day. The stats paint a clear picture: 57.89% of emergency department doctors experience burnout, making them the most stressed healthcare professionals in the field. This isn't just about tired doctors—it's about a system that's breaking down.
Think about Dr. Sarah's typical shift at Metro General's emergency department. She sees 25 patients in 12 hours, from heart attacks to broken bones. Between each patient, she races to update electronic health records. The average emergency physician spends 6.82 minutes on EHR tasks per patient encounter. That's over two hours of pure documentation time during a single shift.
The problem gets worse when you break down the numbers. Emergency doctors spend 3.72 minutes documenting each patient visit, compared to just 1.05 minutes reviewing patient records. In other words, they spend nearly four times more energy writing notes than actually reading important patient information.
This documentation burden creates a dangerous cycle. Rushed notes lead to incomplete records. Incomplete records create legal risks. Legal risks force doctors to spend even more time on paperwork. Meanwhile, patients wait longer for care, and physician burnout reaches crisis levels.
How AI Medical Scribes Transform Emergency Care
AI medical scribes work like having a super-smart assistant who never gets tired, never takes breaks, and never makes spelling mistakes. These systems listen to doctor-patient conversations and automatically create detailed medical notes in real-time.
Here's how it works in practice: Dr. Martinez examines a patient with chest pain. As she asks questions and performs tests, the AI scribe captures every important detail. It notes the patient's symptoms, medical history, vital signs, and treatment plan. By the time Dr. Martinez finishes her examination, a complete, accurate note is ready for her review.
The results speak for themselves. Healthcare facilities using AI scribes report documented time savings of up to 75% in their emergency departments. This isn't just about efficiency—it's about giving doctors their lives back.
Emergency departments that implement AI scribes see immediate improvements in workflow. Consider Valley Medical Center, which installed AI scribes in their emergency department last year. Within three months, their physicians reported feeling less stressed and more connected to patient care. The AI handled the paperwork while doctors focused on healing.
Emergency Department AI Scribing Tools—Comparison Table
While multiple AI scribing solutions exist, emergency departments need tools specifically designed for acute care settings with rapid patient turnover.
The comparison reveals key differences that matter in emergency settings. ScribeHealth stands out with its emergency department focus and lightning-fast setup time. While other solutions treat emergency medicine as just another specialty, ScribeHealth builds its entire platform around the unique needs of acute care.
Speed matters most in emergency departments. When a trauma patient arrives, doctors need documentation that keeps pace with rapid-fire decisions. ScribeHealth's real-time processing means notes appear instantly, not minutes later when the moment has passed.
Emergency departments also need comprehensive comparison tools that understand the difference between routine check-ups and life-threatening emergencies. ScribeHealth's emergency-specific training helps it recognize urgent terminology, critical procedures, and time-sensitive documentation requirements.
AI Documentation Healthcare Tools: How Do They Work in the ED?
Understanding the technical capabilities of AI scribes in high-pressure emergency environments helps clinicians make informed implementation decisions.
Real-Time Documentation Capture
AI documentation healthcare systems work by listening to natural conversations between doctors and patients. Think of it like having a medical school graduate who never sleeps, sitting quietly in the corner of your exam room, taking perfect notes every time.
The technology uses advanced speech recognition to capture medical terminology, patient symptoms, and treatment decisions. Unlike generic voice-to-text software, these systems understand medical language. They know the difference between "chest pain" and "chest pain radiating to the left arm." They recognize when you say "normal saline" versus "normal patient."
Most importantly, these clinical documentation AI tools work in real-time. As you examine a patient with abdominal pain, the system captures your assessment, differential diagnosis, and treatment plan instantly. By the time you finish your examination, a complete note waits for your review and approval.
The system doesn't just transcribe your words—it organizes them into proper medical documentation format. It creates structured SOAP notes with clear sections for subjective complaints, objective findings, assessments, and plans. This saves you from reformatting scattered voice notes into coherent medical records.
Integration with Emergency Department Workflows
Modern AI medical scribes integrate seamlessly with existing emergency department systems. They connect directly to your electronic health record through secure APIs, eliminating the need for copy-and-paste workflows that create documentation errors.
The integration process typically takes 24-48 hours, not weeks of system downtime. Your IT team works with the AI scribe provider to establish secure connections that meet all HIPAA compliance requirements. Patient data never leaves your hospital's secure network, maintaining the privacy standards your emergency department demands.
Here's how it works in practice: Dr. Johnson sees a motorcycle accident victim. As she documents the patient's injuries and treatment plan, the AI scribe automatically populates the trauma flowsheet. The system knows which fields need completion for trauma documentation and ensures nothing gets missed during the controlled chaos of emergency care.
The AI also handles routine tasks that slow down emergency workflows. It can automatically generate billing codes based on documented procedures, create discharge instructions that match your hospital's protocols, and even flag potential medication interactions before they become problems.
Critical Note Components for Emergency Care
Emergency medicine documentation requires specific elements that other medical specialties don't need. The AI scribe must capture time-sensitive information like arrival times, triage levels, and pain scale assessments. It needs to document rapid decision-making processes and changing patient conditions.
Consider the complexity of documenting a cardiac arrest resuscitation. The AI scribe tracks medication dosages, defibrillation attempts, rhythm changes, and time intervals between interventions. It creates a timeline that emergency physicians can use for quality improvement and legal protection.
The system also understands emergency medicine's unique documentation requirements. It knows to capture Glasgow Coma Scale scores, trauma team activation criteria, and procedures like intubation or chest tube insertion. This comprehensive capture ensures your notes meet both clinical and legal standards.
Research shows that emergency physicians currently spend 50% of their documentation time can be reduced through AI scribes. This massive time savings allows physicians to focus more energy on patient care and less on administrative tasks.
Why Choose ScribeHealth for Automated Emergency Department Documentation?
ScribeHealth's emergency department focus and proven track record make it the ideal solution for high-volume, time-sensitive clinical environments.
Emergency-Optimized Features
ScribeHealth wasn't built as a general medical transcription tool that happens to work in emergency departments. It was designed from the ground up specifically for AI medical scribe for emergency departments use cases. This focus shows in every feature and function.
The platform recognizes emergency medicine terminology that other systems miss. It understands phrases like "fast exam negative" and "STEMI alert activated." It knows the difference between chest pain protocols and abdominal pain workups. This specialized knowledge creates more accurate, clinically relevant documentation.
ScribeHealth also handles the rapid pace of emergency care better than generic solutions. When you're managing multiple patients simultaneously, the system tracks each conversation separately. It won't mix up Patient A's chest pain with Patient B's leg fracture, even when you're discussing both cases within minutes of each other.
The emergency-specific templates save additional time. Instead of starting with blank documentation, you get pre-populated forms that match common emergency presentations. The system knows that chest pain evaluations need EKG findings, cardiac enzyme results, and risk stratification scores. It prompts you for these elements automatically.
Rapid Implementation and Training
Emergency departments can't afford lengthy implementation periods that disrupt patient care. ScribeHealth's streamlined setup process gets your team up and running in days, not months.
The training process recognizes that emergency physicians learn differently than other specialists. You need hands-on experience with real patient scenarios, not classroom lectures about theoretical use cases. ScribeHealth provides simulation-based training that mirrors actual emergency department workflows.
Your staff can practice with the system using mock patient encounters before going live. This approach builds confidence and prevents the learning curve from affecting patient care quality. Within 48 hours, most emergency physicians feel comfortable using the system independently.
The platform also provides increased patient capacity benefits almost immediately. As documentation time decreases, physicians can see more patients without working longer hours. This improved efficiency helps reduce emergency department crowding and improves patient satisfaction scores.
24/7 Support for Round-the-Clock Care
Emergency departments never close, and neither does ScribeHealth's support team. Unlike other AI scribe providers that offer business-hours support, ScribeHealth provides round-the-clock technical assistance that matches your schedule.
When technical issues arise at 2 AM during a busy Saturday night shift, you can't wait until Monday morning for help. ScribeHealth's support team includes emergency medicine professionals who understand the urgency of your needs. They can troubleshoot problems quickly and get your documentation system back online.
The investment in AI medical scribes continues growing rapidly. The market saw $800 million in AI scribe funding in 2024, doubled from $390 million in 2023. This massive investment reflects the healthcare industry's confidence in AI scribing technology and its potential to solve documentation challenges.
Currently, 60 AI scribe solutions operate across healthcare, but ScribeHealth's emergency department specialization sets it apart from general-purpose competitors. While other companies chase multiple market segments, ScribeHealth maintains laser focus on emergency medicine's unique needs.
FAQs About Emergency Department AI Scribing Tools
Common questions about AI scribe implementation in emergency departments address concerns about accuracy, integration, and workflow disruption.
Accuracy and Reliability Questions
Q: How accurate are AI scribes in noisy emergency departments?
ScribeHealth maintains accuracy rates above 95% even in high-noise environments. The system uses advanced filtering technology to focus on physician voices while filtering out background sounds like monitors, conversations, and equipment alarms.
Q: What happens if the AI makes a mistake?
Every AI-generated note requires physician review and approval before entering the medical record. The system highlights any uncertain phrases for your attention, and you maintain complete control over the final documentation. Training requirements include learning how to quickly review and edit AI-generated content.
Integration and Workflow Concerns
Q: Will AI scribes slow down my workflow during busy shifts?
The opposite typically occurs. Emergency departments using medical scribing software report smoother workflows because physicians spend less time on computers and more time with patients. The AI works in the background, creating documentation without interrupting your natural examination process.
Q: How quickly can we implement the system?
ScribeHealth's emergency medicine AI implementation typically takes 24-48 hours for technical setup, followed by brief training sessions. Most emergency departments go live within one week of initial contact.
Cost and Implementation Timeline
Q: Is AI scribing cost-effective for smaller emergency departments?
Industry experts predict 30% of healthcare facilities will adopt AI scribes by the end of 2025, indicating broad market acceptance across facility sizes. At $49 per month per physician, ScribeHealth typically pays for itself through improved efficiency and reduced overtime costs.
Conclusion—Turn the Pressure of Emergency Documentation Into Precision, with ScribeHealth
Emergency medicine pushed you to your limits, but documentation doesn't have to. ScribeHealth transforms the biggest source of physician burnout into your competitive advantage. While other emergency departments struggle with paperwork, you'll focus on what matters most—exceptional patient care.
Your patients deserve your full attention, not half your focus while the other half worries about documentation. ScribeHealth gives you that freedom back. Join the thousands of emergency physicians who've already discovered how AI scribes restore the joy of practicing medicine.
Ready to eliminate documentation stress forever? Book a demo with ScribeHealth today and experience the difference 24 hours can make in your emergency department.

