Transform Your Medical Billing: Automation Strategies That Actually Work
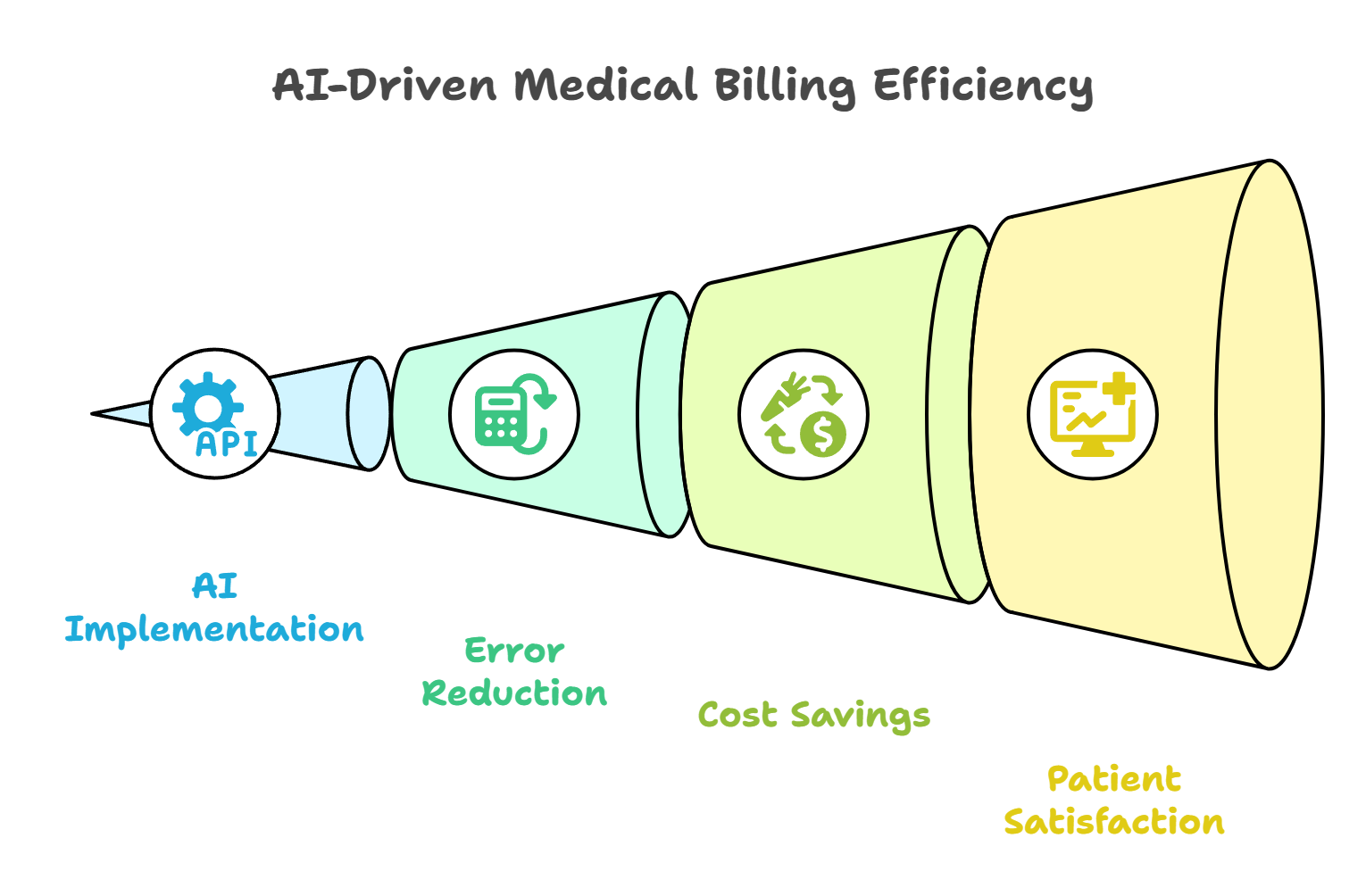
Medical practices waste thousands on billing errors and frustrated patients. AI-powered billing automation cuts errors by 90% and speeds up payments by 50%. This guide shows you how to automate your workflow, reduce costs, train staff, and create happier patient experiences while boosting your revenue.

Manual billing mistakes cost practices thousands of dollars every month. Patient complaints about confusing bills hurt your reputation. Staff spend too much time on repetitive tasks instead of helping patients. AI-based medical billing solutions can reduce billing errors by up to 90%. This guide shows you how to automate your billing process, cut costs, and make patients happier with their billing experience.
The Hidden Costs of Manual Billing in Modern Medical Practices
Manual billing processes continue to drain practice resources and compromise patient relationships, but the true scope of this challenge extends far beyond simple data entry errors.
Financial Impact of Billing Inefficiencies
Every denied claim costs your practice money. When staff enter the wrong codes or miss important details, insurance companies reject claims. This means you wait longer to get paid for your services.
Think about a typical family practice. If they submit 100 claims per week and 20% get denied due to errors, that's 20 claims that need to be fixed and resubmitted. Each rework costs time and money. Some practices lose thousands of dollars monthly just from preventable billing mistakes.
AI implementation in medical billing can decrease claims processing time by 50%. This faster processing means you get paid quicker. When claims go through on the first try, your cash flow improves dramatically.
Staff overtime adds another hidden cost. When billing teams work late to fix errors or catch up on paperwork, you pay extra wages. Many practices don't realize how much these overtime hours cost them each year.

Patient Experience Consequences
Billing problems hurt patient relationships more than most practices realize. Confusing bills, surprise charges, and payment delays frustrate patients. When patients don't understand their bills, they call your office repeatedly for explanations.
90% of patients say loyalty relies on their financial (billing) experience. This means billing mistakes can make patients leave your practice. Losing just one patient family can cost thousands in future revenue.
Consider Sarah, a working mom who receives a confusing medical bill with unclear charges. She spends her lunch break calling the billing office three times to understand what she owes. This frustrating experience makes her think about finding a new doctor next time.
Poor billing experiences also hurt your online reputation. Patients often mention billing problems in online reviews. These negative reviews can drive away new patients before they even visit your practice.
Physician Billing Automation Workflow Optimization: Core Components
Modern automated billing systems transform every step of the revenue cycle, from initial patient contact through final payment posting, creating seamless workflows that reduce errors and accelerate cash flow.
Eligibility Verification Automation
Automated eligibility verification checks if patients have valid insurance before their appointments. The system connects directly to insurance company databases in real-time. This prevents surprises on the day of service.
For example, when Mary schedules an appointment online, the system automatically checks her insurance status. If her coverage expired, the system alerts her immediately. This gives Mary time to update her insurance or discuss payment options before her visit.
Real-time verification also helps your front desk staff. They don't need to call insurance companies or wait on hold. The system does this work automatically, freeing staff to help patients with other needs.
Some advanced systems even send automated messages to patients about their coverage. If someone's insurance changes, they get a text reminder to bring their new card to their appointment.
Intelligent Charge Capture
Smart charge capture systems pull billing information directly from your electronic health records (EHR). When a doctor documents a patient visit, the system automatically identifies billable services. This reduces the chance of missing charges or using wrong codes.
Think of it like a smart shopping receipt. Instead of manually writing down each item, the system scans what happened during the visit and creates the bill automatically. This process is much faster and more accurate than manual entry.
AI Scribing 101: What You Need to Know explains how modern AI systems help with documentation. These tools work together with billing automation to create seamless workflows.
The system also suggests the most accurate billing codes based on the medical documentation. If a doctor treated a patient for high blood pressure and diabetes, the system recommends the right codes for both conditions.
AI-Powered Claim Scrubbing & Submission
Before sending claims to insurance companies, automated systems check them for errors. This process is called claim scrubbing. These automated medical billing error reduction strategies look for missing information, wrong codes, or other problems that cause denials.
Imagine having a proofreader who never gets tired and checks every detail. That's what automated claim scrubbing does for your billing. It catches mistakes before they become expensive problems.
The system compares each claim against insurance company rules. Different insurers have different requirements, and keeping track of all these rules is impossible for humans. But automated systems stay updated with the latest requirements from hundreds of insurance companies.
When the system finds a problem, it alerts your billing staff immediately. Staff can fix the issue before sending the claim, which means faster payments and fewer headaches.
Automated Payment Posting & Reconciliation
When insurance companies pay claims, they send electronic remittance advice (ERA) files. These files contain payment details for multiple claims. Manual processing of these files takes hours and often leads to posting errors.
Automated systems read ERA files instantly and post payments to the correct patient accounts. The system matches payments to the right claims automatically. This eliminates the tedious work of manually entering each payment.
For example, if Blue Cross pays $150 for John's office visit, the system automatically credits his account. It also updates your financial reports in real-time. Your practice always knows exactly how much money you've collected each day.
The system also handles partial payments and adjustments. If an insurance company pays less than expected, it flags the difference for review. This helps your team catch underpayments quickly.
Intelligent Denial Management
Some claims still get denied even with perfect automation. Smart denial management systems analyze why claims get rejected. They look for patterns and suggest ways to prevent future denials.
Automated billing process reduced manual errors by 30% and increased patient satisfaction scores by 20% within six months. This improvement comes from catching problems before they become denials.
The system can automatically generate appeals for common denial reasons. If Medicare denies a claim for "insufficient documentation," the system pulls the required medical records and creates an appeal letter. This saves hours of manual work.
Pattern recognition helps prevent future problems. If the system notices that certain procedure codes always get denied by a specific insurer, it alerts your team. You can then verify requirements before submitting similar claims.
Patient Billing & Communication Automation
Automated patient billing creates clear, easy-to-understand statements. Instead of confusing medical codes, patients see plain English descriptions of their services. The system also shows how much insurance paid and what the patient owes.
Smart payment reminders use multiple channels to reach patients. The system might send an email reminder one week after the bill, followed by a text message if payment isn't received. This gentle approach is more effective than aggressive collection calls.
Patients can access self-service portals to view their bills, make payments, and set up payment plans. These portals work 24/7, so patients can handle their billing needs anytime. This convenience reduces calls to your billing office.
For patients who need payment plans, the system can automatically offer options based on the bill amount. A $500 bill might trigger an offer for a 3-month payment plan, while a $2,000 bill might offer 6 or 12 months.
Physician Practice Billing Automation Benefits: ROI Analysis
The financial and operational advantages of billing automation extend far beyond simple cost savings, creating compound benefits that transform practice efficiency and growth potential.
Revenue Optimization
Faster claim submission means quicker payments. When claims go out the same day as patient visits, you get paid weeks sooner. This improved cash flow helps with daily operations and reduces the need for expensive credit lines.
Automated systems also catch more billable services. Manual processes often miss procedures or supplies that should be billed. Smart charge capture ensures you bill for everything you provide.
Consider Dr. Johnson's family practice. Before automation, they missed billing for about 5% of vaccinations given during routine visits. With automated charge capture, they now bill for 100% of services. This added $30,000 to their annual revenue.
Cost Reduction Strategies
AI-enabled billing systems can reduce administrative costs by up to 30%. This savings comes from needing fewer billing staff and reducing overtime costs.
Automation also reduces training costs. New employees can learn automated systems faster than complex manual processes. When staff leave, replacements get up to speed quickly.
Error reduction saves money in unexpected ways. Fewer denied claims mean less staff time spent on rework. Your team can focus on more valuable tasks like patient care coordination or practice improvement projects.
Compliance costs also decrease with automation. The system stays updated with changing regulations automatically. You don't need to send staff to expensive training sessions or hire consultants to interpret new rules.
Operational Efficiency Gains
Staff productivity improves dramatically with automation. Billing clerks can process twice as many claims in the same time. This increased efficiency lets you handle more patients without hiring additional staff.
Boosting Productivity with AI Medical Scribe Automation explains how automation helps entire practice workflows. These efficiency gains compound over time.
Reduced burnout is another important benefit. When staff don't spend hours on repetitive data entry, they feel more satisfied with their jobs. Lower turnover saves money on recruiting and training new employees.
Automation also improves work-life balance. Staff can finish their work during regular hours instead of staying late to catch up on billing tasks. Happy employees provide better patient service.
Automated Billing System Training for Medical Staff: Best Practices
Successful automation implementation relies heavily on comprehensive staff training that addresses both technical competencies and change management, ensuring smooth adoption across all practice roles.
Role-Based Training Strategies
Different staff members need different types of training. Front-desk workers focus on patient registration and insurance verification. Billing specialists learn advanced features like denial management and reporting. Clinical staff need to understand how their documentation affects billing.
Start with your front-desk team. They need to know how the new system checks insurance eligibility and registers patients. Show them how automated alerts help catch problems before patients arrive. Practice common scenarios like expired insurance cards or incorrect patient information.
Billing staff training goes deeper into system features. They learn how to review automatically generated claims, handle exceptions, and run reports. Focus on how automation changes their daily tasks rather than replacing them entirely.
Change Management & Staff Buy-In
Some staff members worry that automation will eliminate their jobs. Address these concerns directly by explaining how automation makes their work easier, not unnecessary. Show specific examples of how the system handles boring, repetitive tasks so staff can focus on more interesting work.
Share success stories from other practices. When employees hear how automation helped similar practices reduce overtime and stress, they become more excited about the changes. Create champions among your staff who can help train and encourage others.
Regular feedback sessions help identify problems early. Ask staff what they like about the new system and what confuses them. Use this feedback to adjust training and improve processes.
Celebrate small wins along the way. When the system prevents a claim denial or speeds up payment posting, recognize the staff members involved. This positive reinforcement helps build enthusiasm for the new processes.
Ongoing Support Systems
Training doesn't end after the initial implementation. Set up help desk support for when staff have questions. This might be an internal expert or access to vendor support during business hours.
Create user manuals and quick reference guides specific to your practice. Generic vendor documentation often doesn't match your exact workflows. Customize guides to show your specific processes and procedures.
Schedule refresher training sessions every few months. As staff become more comfortable with basic features, they can learn advanced capabilities. Regular training also helps when you hire new employees.
Video tutorials work well for ongoing support. Staff can watch specific procedures when they need reminders. These videos are especially helpful for training new hires or covering less common tasks.
Medical Practice Automated Billing Implementation Guide: Step-by-Step Process
A systematic approach to implementation ensures minimal disruption to daily operations while maximizing the benefits of automation from day one.
Pre-Implementation Assessment
Before choosing any system, analyze your current billing workflow. Document every step from patient registration through final payment. Identify bottlenecks where work piles up or errors commonly occur.
Calculate your current costs including staff salaries, overtime, and error-related expenses. This baseline helps measure return on investment later. Also track key metrics like days in accounts receivable and first-pass claim approval rates.
Survey your staff about current pain points. They often know exactly where problems occur and have ideas for improvements. This input helps you prioritize which features matter most for your practice.
Review your current technology infrastructure. Make sure your computers, internet connection, and EHR system can support new billing software. Outdated technology might need upgrades before implementation.
System Selection & Vendor Evaluation
Look for systems that integrate well with your existing EHR. Seamless integration prevents double data entry and reduces errors. The billing system should pull patient and procedure information directly from your medical records.
Test the system with real scenarios from your practice. Most vendors offer demos or trial periods. Use actual patient cases to see how well the system handles your specific needs.
Evaluate vendor support options. Good vendors provide training, ongoing support, and regular system updates. Ask about response times for technical issues and availability of phone support during your business hours.
Data Migration & Integration Planning
Moving data from your old system requires careful planning. Create a complete backup of all current data before starting. Test the migration process with a small amount of data first to identify potential problems.
Map data fields between your old and new systems. Patient names and addresses usually transfer easily, but custom fields might need special handling. Work with your vendor to ensure all important information transfers correctly.
Plan for data cleanup during migration. This is a good time to fix duplicate patient records, update old addresses, and standardize procedure codes. Clean data makes the new system work better from day one.
Schedule migration during slow periods if possible. Weekend conversions work well for many practices. This gives you time to test everything before patients arrive on Monday morning.
Phased Rollout Strategy
Start with one part of your billing process rather than changing everything at once. Many practices begin with eligibility verification because it's simple and shows immediate benefits.
Train a small group of super users first. These employees become internal experts who can help train others. Choose staff members who adapt well to change and enjoy learning new technology.
Set realistic timelines for each phase. Rushing implementation leads to mistakes and frustrated staff. Allow extra time for training and adjustments during the first few weeks.
Monitor key performance indicators throughout the rollout. Track metrics like claim approval rates, processing times, and staff satisfaction. This data helps you identify and fix problems quickly.
Go-Live Support & Optimization
Have extra support available during the first week of full implementation. This might include vendor representatives on-site or extended help desk hours. Quick problem resolution prevents small issues from becoming major headaches.
Continue measuring performance after go-live. Compare new metrics to your baseline measurements to quantify improvements. Share these results with staff to maintain enthusiasm and identify areas for further improvement.
Schedule regular optimization reviews. Most systems have features you won't use immediately. As staff become comfortable with basic functions, gradually introduce advanced capabilities that can provide additional benefits.
Patient-Friendly Automated Billing Experience Design
Modern patients expect transparency, convenience, and clear communication in their billing interactions, making patient experience design a critical component of successful automation.
Clear Communication Strategies
Replace medical codes with plain English descriptions on patient statements. Instead of "99213," show "Office visit for established patient." This simple change eliminates confusion and reduces billing questions.
Include visual elements like charts or graphs to show insurance payments versus patient responsibility. A simple pie chart showing "Insurance paid $200, You owe $50" is much clearer than lines of text with numbers.
Provide upfront cost estimates whenever possible. When patients schedule procedures, the system can estimate their out-of-pocket costs based on their insurance benefits. This transparency builds trust and reduces surprise bills.
Send appointment reminders that include estimated costs. For example: "Your appointment tomorrow is confirmed. Based on your insurance, your estimated cost is $25-40." This helps patients plan and brings payment cards to their visit.
Multiple Payment Options & Convenience
Online payment portals let patients pay bills anytime. Include options for credit cards, debit cards, and electronic bank transfers. Make the payment process simple with just a few clicks.
Mobile-friendly payment options are essential. Many patients prefer to handle bills on their phones during lunch breaks or while commuting. Ensure your payment system works well on smartphones and tablets.
Offer payment plans automatically for larger bills. The system can suggest monthly payment options based on the total amount. For a $600 bill, it might offer 3, 6, or 12-month payment plans with clear monthly amounts.
Text message payment reminders work well for younger patients. A simple text saying "Your $45 bill is due in 3 days. Pay now at [link]" is convenient and effective. Always include opt-out options for patients who prefer other communication methods.
Self-Service Capabilities
Patient portals should show complete billing history, not just current balances. Patients want to see what services they received, when insurance paid, and how balances changed over time.
Let patients update their insurance information through the portal. When someone gets a new job or changes insurance, they can upload new card images and update their information without calling your office.
Include explanation of benefits (EOB) information in the portal. When patients see exactly what insurance covered and why, they understand their bills better. This reduces confusion and phone calls to your billing office.
Provide easy access to billing support through the portal. Include frequently asked questions, contact information, and even chat features for quick questions. This gives patients options for getting help without phone calls.
Medical Billing AI User Experience Optimization
AI-enhanced billing systems provide intelligent insights and predictive capabilities that transform how billing teams work and make decisions.
Intelligent Dashboard Features
Modern billing dashboards show personalized insights for each team member. Billing specialists see claims that need attention, while managers see overall practice performance. This customization helps everyone focus on their most important tasks.
Real-time metrics help teams stay on track throughout the day. Dashboards might show claims submitted, payments received, and denials that need work. Teams can see their progress and adjust priorities as needed.
Predictive analytics help with cash flow planning. The system analyzes historical patterns to predict when payments will arrive. This helps practices plan expenses and manage cash flow more effectively.
Automated alerts notify staff about important events. If a large claim gets denied or a payment is delayed, the system sends immediate notifications. Quick responses to problems prevent small issues from becoming major headaches.
Natural Language Processing Applications
AI systems can read medical notes and suggest appropriate billing codes. When a doctor writes "patient has high blood pressure and diabetes," the system recommends codes for both conditions. This reduces coding errors and ensures complete billing.
Automated coding suggestions learn from your practice patterns. If your cardiologist always uses specific codes for certain procedures, the system learns these preferences. Over time, suggestions become more accurate and relevant.
The system can also flag unusual patterns for review. If coding suddenly changes for a specific provider or procedure, it alerts billing staff to double-check the documentation. This quality control prevents errors before claims go out.
Continuous Learning & Adaptation
AI systems improve over time by learning from claim outcomes. When claims get approved quickly, the system notes successful patterns. When claims get denied, it learns what to avoid in similar situations.
Automatic updates keep the system current with changing regulations. New billing rules, updated procedure codes, and payer requirement changes get incorporated automatically. Your team doesn't need to track these changes manually.
The system adapts to each payer's specific requirements. Different insurance companies have different rules and preferences. AI learns these patterns and adjusts claim formatting accordingly for better approval rates.
Performance feedback helps the system make better suggestions. When staff override AI recommendations, the system learns from these decisions. This continuous improvement makes the AI more helpful over time.
Automated Medical Billing Error Reduction Strategies
Systematic error prevention through automation creates more reliable billing processes while reducing the manual oversight traditionally required for quality assurance.
Real-Time Validation Systems
Pre-submission claim scrubbing catches errors before they cause denials. The system checks every claim against insurance company rules and requirements. Problems get flagged immediately for correction.
Coding accuracy verification ensures the right codes are used for each service. The system compares procedure codes with diagnosis codes to make sure they match logically. It also checks for missing or duplicate codes.
Duplicate detection prevents double billing for the same service. If someone accidentally enters the same procedure twice, the system catches it before submission. This protects your practice from fraud accusations and payment clawbacks.
Real-time insurance verification prevents eligibility problems. The system checks patient coverage immediately when appointments are scheduled. This catches expired policies or coverage changes before services are provided.
Pattern Recognition & Analytics
The system analyzes denial trends to identify recurring problems. If specific procedure codes always get denied by certain insurers, it alerts your team. You can then research requirements and prevent future denials.
Proactive issue identification helps fix problems before they spread. If the system notices increasing denials for a specific provider, it can flag recent changes in documentation or coding patterns.
Compliance monitoring ensures your practice follows all regulations. The system tracks billing patterns and alerts you to anything that might look suspicious to auditors. This proactive approach prevents compliance problems.
Performance analytics show which areas need improvement. You can see denial rates by provider, procedure type, or insurance company. This data helps you focus training and improvement efforts where they're needed most.
Audit Trail & Transparency
Complete change tracking records every modification to billing data. If someone changes a procedure code or patient information, the system logs who made the change and when. This detailed history helps with audits and dispute resolution.
Compliance documentation automatically generates reports for auditors. The system can produce detailed records showing how claims were processed, what checks were performed, and who approved each step.
Performance reporting tracks quality metrics over time. You can see trends in error rates, processing times, and staff productivity. This data helps demonstrate continuous improvement to auditors and accreditation bodies.
Measuring Success: KPIs and Performance Metrics
Establishing clear success metrics ensures that automation investments deliver measurable improvements in both financial performance and operational efficiency.
Financial Performance Indicators
Days in accounts receivable measures how quickly you collect payments. Before automation, practices often wait 45-60 days for payment. Good automated systems reduce this to 25-35 days, significantly improving cash flow.
First-pass claim approval rates show billing accuracy. Manual processes typically achieve 75-85% first-pass approval. Automated systems often reach 95% or higher, reducing rework and speeding payments.
Collection percentages track how much of billed amounts you actually collect. Automation helps by reducing billing errors, improving patient communication, and making payments more convenient.
Net collection rates factor in contractual adjustments and write-offs. This metric shows the true effectiveness of your revenue cycle. Automation typically improves net collection rates by 2-5 percentage points.
Operational Efficiency Metrics
Staff productivity measures how many claims each employee processes per day. Automation typically doubles or triples productivity, allowing the same staff to handle more volume or freeing time for other tasks.
Error rates track billing accuracy improvements over time. Measure both internal errors caught before submission and external denials from payers. Both should decrease significantly with good automation.
Patient satisfaction scores often improve with automated billing. Clearer statements, convenient payment options, and faster problem resolution lead to happier patients. Track billing-related complaints and compliments.
Time-to-resolution measures how quickly billing problems get fixed. Automated systems help staff identify and resolve issues faster, improving both patient satisfaction and cash flow.
Continuous Improvement Strategies
Regular performance reviews help optimize system settings and workflows. Schedule monthly meetings to review metrics and identify improvement opportunities. Small adjustments can lead to significant gains over time.
Staff feedback provides insights that metrics might miss. Ask employees what's working well and what could be better. They often have practical suggestions for improving efficiency.
Benchmark against industry standards to see how your practice compares. Many professional organizations publish average performance metrics. Use these benchmarks to set realistic improvement goals.
System optimization protocols ensure you're getting full value from your automation investment. Work with your vendor to implement new features and fine-tune existing processes for better results.
FAQs – People Also Ask
Is there an AI for medical billing?
Yes, several AI-powered platforms automate medical billing tasks. These systems can extract billing data from clinical notes, recommend appropriate codes, validate claims before submission, and even predict which claims might get denied.
AI billing systems work by reading medical documentation and translating it into billing codes. They check claims against insurance company rules and catch errors before submission. Some advanced systems can even generate appeals for denied claims automatically.
Many practices report significant improvements with AI billing systems. They see fewer denials, faster payments, and reduced staff workload. The technology continues to improve as AI learns from more billing data.
How can AI be used for billing?
AI helps with billing in several ways. It can read doctor's notes and suggest billing codes automatically. It checks claims for errors before sending them to insurance companies. It can also predict payment patterns and identify potential collection problems.
Natural language processing lets AI understand medical documentation written in normal English. Machine learning helps the system improve over time by learning from successful and unsuccessful claims.
AI can also automate patient communications like payment reminders and billing explanations. It personalizes messages based on patient preferences and payment history for better results.
Can you automate medical billing?
Absolutely. Modern billing systems can automate most steps from eligibility verification through payment posting. The level of automation depends on your current technology and how much you want to automate.
Most practices start with basic automation like eligibility checking and claim submission. As staff become comfortable, they add more advanced features like automated payment posting and denial management.
Complete automation isn't always the goal. Many practices prefer to automate routine tasks while keeping human oversight for complex cases. This hybrid approach combines efficiency with flexibility.
Conclusion – The Future of Physician Billing is Automated
Physician billing automation represents a fundamental shift toward more efficient, accurate, and patient-centered healthcare administration that every modern practice must embrace.
The evidence is clear: automated billing systems deliver measurable improvements in revenue, efficiency, and patient satisfaction. Practices that implement these systems see fewer errors, faster payments, and happier staff. More importantly, they can focus more time and energy on patient care instead of administrative tasks.
The technology will only get better. AI systems continue learning and improving, making billing even more accurate and efficient. Early adopters gain competitive advantages that compound over time. Patients increasingly expect the convenience and transparency that modern billing systems provide.
.png)
